Think about the last time you were forced to make a decision in the face of uncertainty. You may have been choosing which job offer to accept or whether to move from renting to buying a home. You probably weighed the tradeoffs and asked yourself whether it made sense to gather additional information or to decide based on the available facts. But waiting for the "perfect" amount of insight has its own opportunity cost — the time that could have accrued positive returns from the investment. On the other hand, making an early decision with greater uncertainty may force you to reevaluate or course correct as new information becomes available.
Government regulators around the world — including the FDA — face similar challenges when making decisions about approving new medicines, weighing the safety and effectiveness based on the information available at the time. Context also factors into approval decisions, with regulators typically calibrating the level of data they require with the need to accelerate access for patients that lack effective treatments. Regulators' decisions aren't static. Over time, as more is learned about drugs through clinical studies and routine use in larger numbers of patients, they may identify safety issues that call for changes to how the drugs are used. When this happens, regulators may issue physicians' alerts or change drug labels. While the regulators can communicate recommendations, the system only works if clinicians modify their behavior based on these regulatory recommendations.
In order for this to work, the information has to be communicated by government regulators effectively and physicians need to be attuned and agile enough to change practice patterns based on recommended modifications. In the US, the FDA is not mandated to track whether their evolving feedback is being used by physicians to inform their decisions. As a result, it is challenging to have real-time transparency into practice patterns and hard to assess whether the patterns were changing in response to updated regulatory guidance.
Our team of researchers wanted to see if physicians in the US have shown the ability to adapt quickly to updated FDA decisions reflecting novel cancer drugs. To do this, we partnered with the FDA's Oncology Center for Excellence and researchers from the University of Pennsylvania to test the impact of an FDA warning and label change for a case in bladder cancer. The full results can be found today in the Journal of the American Medical Association — read on for a summary of our findings.
We learned that when the FDA first approved the use of immunotherapy drugs for bladder cancer using an accelerated approval approach in 2017, the uptake of these agents, unsurprisingly, began to skyrocket. Many patients, traditionally treated with chemotherapy, saw immunotherapy as an option filled with the hope of better health outcomes and fewer side effects. The new medicine, during this period, was used in first-line treatment for bladder cancer.
But, in May 2018, more information became available to the FDA from two Phase III randomized controlled trials. The results suggested that immunotherapy did not benefit all patients equally. In fact, patients on immunotherapy who lacked a particular biomarker status appeared to do worse than those receiving standard chemotherapy. The FDA soon followed up with an alert , advising practitioners to give it only to patients with this specific biomarker status. Following the announcement, they took quick action to update the drug labels accordingly.
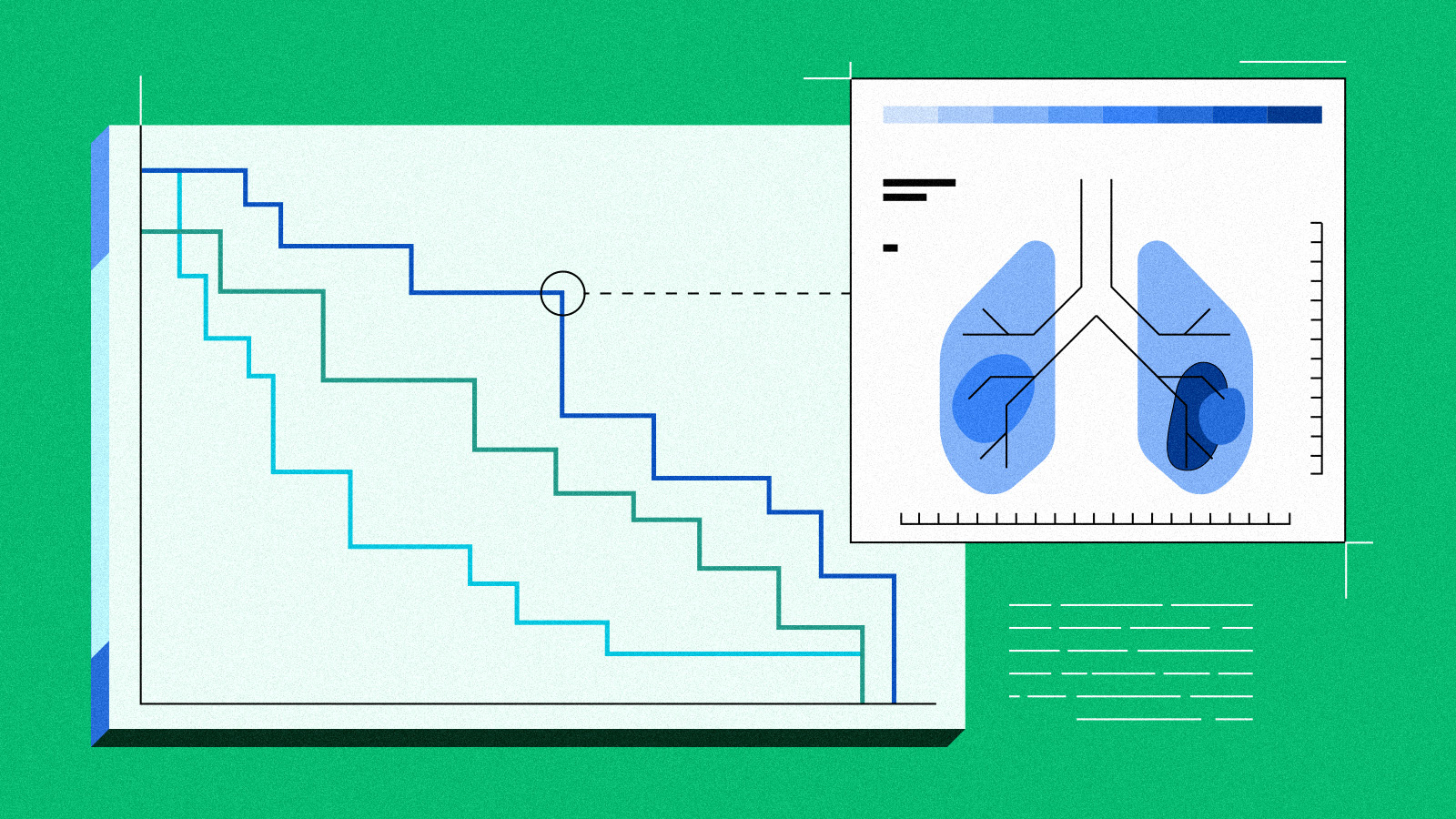
Given this clear before and after change in prescribing information, there was an opportunity to test how physicians changed their behavior in response to this type of guidance. Our team of scientists and oncologists hypothesized that if physicians were listening, and upon effective communication of the FDA's guidance, then we would observe three events beginning in June 2018:
-
The decline of immunotherapy treatment of bladder cancer
-
A corresponding rise in chemotherapy as a substitute therapy
-
A jump in biomarker testing rates, since few of these patients received prior testing
We proposed the study design at the time of the FDA label change and then waited to see what would happen. Six months later, we analyzed the real world data to test our hypotheses. We found that before the warning , everything looked as expected. Chemotherapy use went down, immunotherapy use went up, and biomarker testing was not very common. But upon the announcement of the FDA's alert and subsequent label change, immunotherapy use went down, chemo use went up, and biomarker testing rates jumped up .
For our study team, these results are encouraging and signal that the communication of updated guidance from regulatory authorities is working. It confirms that practitioners — both community oncologists and those practicing in academic medical centers — are in touch with the rapidly changing field of available treatments and approvals, and it means that they care for their patients with the best evidence available. Given the changing landscape of drug approvals, it's challenging to stay current on how things are changing. But this study provides evidence suggesting that the trusting relationship and dynamics between FDA guidances and practicing physicians is working in oncology.